Dayton sciatica is a common neurosurgical condition that affects the sciatic nerve, causing pain, numbness, and weakness in the lower back, hips, and legs. While neurosurgery can be life-saving and life-enhancing, it also poses ethical dilemmas, as the risks and benefits of the procedure must be carefully evaluated and balanced. In this article, we will explore the complex ethical considerations that arise in neurosurgery and discuss how neurosurgeons can navigate these challenges.
Beneficence and Non-Maleficence
Beneficence and non-maleficence are two fundamental ethical principles that guide medical practice. Beneficence refers to the obligation to do good and promote the well-being of the patient, while non-maleficence refers to the obligation to avoid harm and minimize risks. In neurosurgery, these principles are often in tension, as the benefits of the procedure must be weighed against the potential risks and harms.
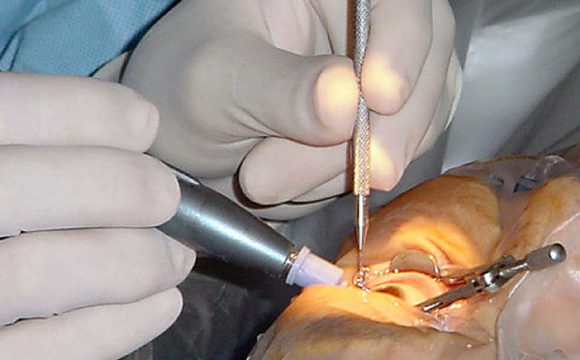
For example, a neurosurgeon may recommend surgery to remove a brain tumor that is causing seizures and impairing cognitive function. While the surgery offers the potential benefit of improving the patient’s quality of life, it also poses risks such as bleeding, infection, and neurological deficits. The neurosurgeon must carefully evaluate the risks and benefits of the procedure and communicate these to the patient, so that the patient can make an informed decision about their treatment.
Informed Consent
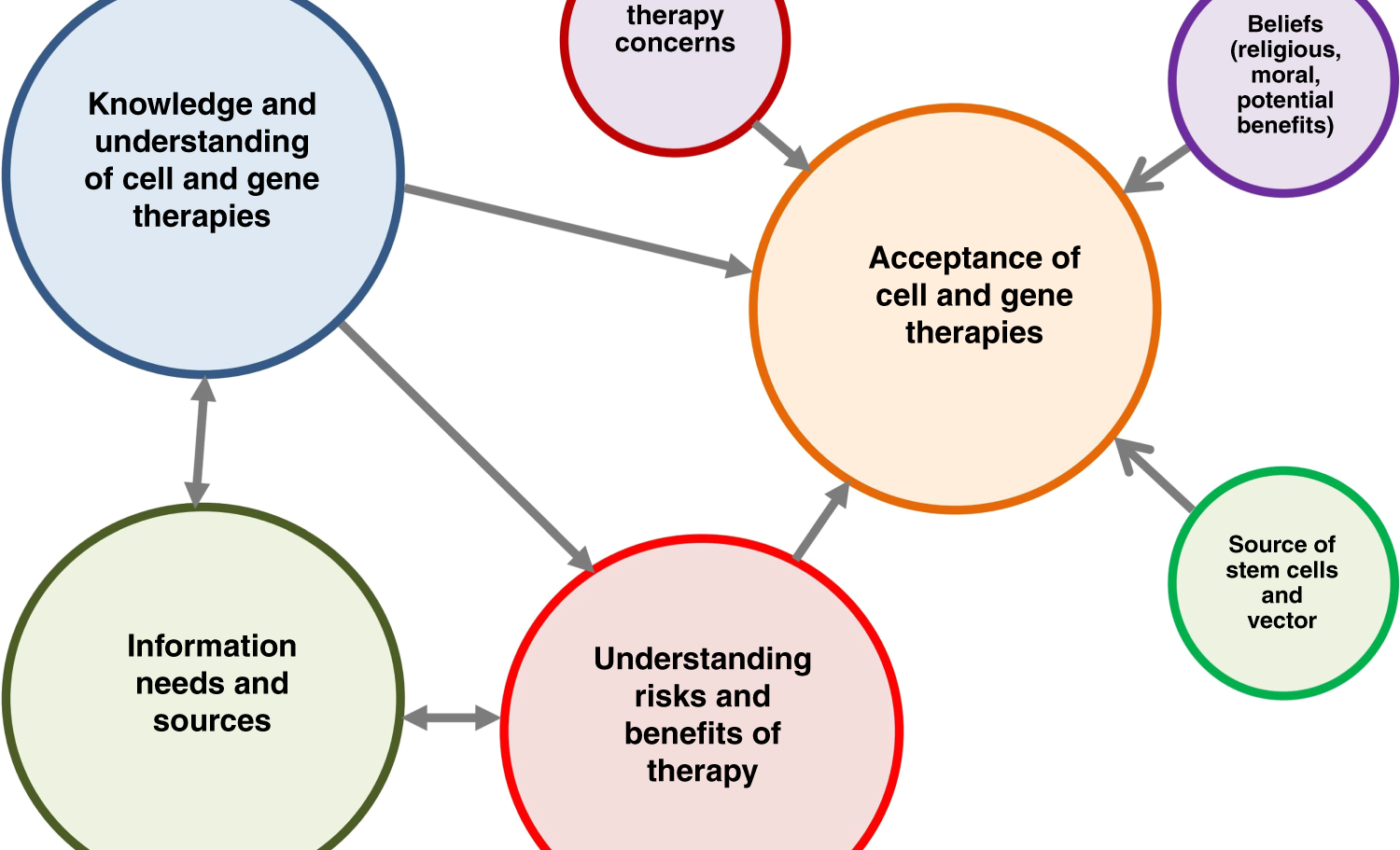
Informed consent is another key ethical consideration in neurosurgery. Informed consent refers to the process by which a patient is fully informed about the risks, benefits, and alternatives to a procedure and gives their voluntary and informed consent to undergo the procedure. In neurosurgery, informed consent is particularly important, as the procedures are often complex and carry significant risks and potential complications.
Neurosurgeons must take the time to explain the nature of the procedure, the rationale for the procedure, the potential risks and benefits, and the alternatives to the procedure to the patient and/or their family members. They must also ensure that the patient understands the information presented and is able to make an informed decision about their treatment. Informed consent is a crucial aspect of respecting patient autonomy and upholding ethical practices in neurosurgery.
Justice and Equity
Justice and equity are two additional ethical principles that guide medical practice. Justice refers to the fair distribution of benefits and burdens, while equity refers to the provision of care that is appropriate to the needs of the patient, regardless of their societal status or background. In neurosurgery, these principles are particularly important, as access to neurosurgical care may be limited due to factors such as geography, socioeconomic status, or insurance coverage.
Neurosurgeons must advocate for equitable access to neurosurgical care and work to address the systemic barriers that prevent patients from receiving the care they need. They must also ensure that the benefits and burdens of neurosurgical procedures are distributed fairly and that all patients have the opportunity to benefit from neurosurgical advances.
Conclusion
Neurosurgery poses complex ethical challenges that require careful consideration and balancing of risks and benefits. Neurosurgeons must uphold the ethical principles of beneficence, non-maleficence, informed consent, justice, and equity in their practice and work to promote the well-being of their patients. By navigating these challenges with sensitivity and expertise, neurosurgeons can provide high-quality care that respects the dignity and autonomy of their patients.